Introduction
Advances in cancer treatment have transformed the landscape in recent years. Among these, immunotherapy has emerged as a powerful tool harnessing the patient’s immune system to attack cancer cells. Under Dr Sudip Shrestha’s leadership at the Nepal Cancer Hospital & Research Center, this modality is being incorporated thoughtfully into oncology practice in Nepal with contexts uniquely adapted to local patients and disease patterns.
What is Immunotherapy?
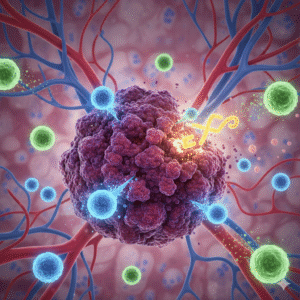
Immunotherapy is a form of cancer treatment that uses the body’s own immune system to recognise, target and destroy malignant cells. While conventional therapies (surgery, radiation, chemotherapy) act directly on the tumour, immunotherapy acts more indirectly by modulating immune mechanisms. The immune system identifies abnormal cells via antigens and other signals; however cancer cells often evade these immune responses. Immunotherapy aims to reverse or bypass these evasion strategies.
Why Immunotherapy Matters
This treatment modality has relevance for patients whose cancers either resist conventional therapies, recur after treatment, or present at an advanced stage. For example, tumours with high mutational burden or expression of specific biomarkers (such as PD-L1) tend to respond better. According to the scientific literature, immunotherapy “has dramatically changed survival and quality of life for many patients” though it remains “in its relative infancy” in many settings. In the context of Nepal, where access to advanced care may be more limited and late presentation is common, the introduction of immunotherapy offers hope but also demands careful selection of patients, infrastructure readiness, and cost‐consideration.
Mechanisms of Action – How Immunotherapy Works
Several mechanisms underlie the therapeutic effect:
- Immune checkpoint inhibition: Certain immune‐checkpoint proteins (such as PD-1, PD-L1, CTLA-4) act as brakes on T-cells; tumours may exploit this to evade immune attack. Blocking these checkpoints can “release the brakes”.
- Adoptive cell therapy / T-cell transfer: Immune cells (often T cells) are harvested, modified and expanded ex-vivo and then reinfused to attack tumour cells.
- Monoclonal antibodies: Laboratory made antibodies bind to specific antigens on tumour cells, making them visible to the immune system or directly triggering immune responses.
- Cancer vaccines and immune system modulators: Vaccines may train the immune system to recognise tumour antigens; cytokines and other modulators may boost immune response.
Modulation of tumour microenvironment: Emerging therapies target the immunosuppressive environment around the tumour to permit effective immune attack.
Applications in Oncology Practice: Insights from Dr Sudip
At the Cancer Hospital in Lalitpur, the integration of immunotherapy reflects a thoughtful strategy:
- Patient selection and biomarker testing
Dr Sudip emphasises testing for relevant biomarkers such as PD-L1 expression, microsatellite instability (MSI), tumor mutational burden (TMB) which help identify which patients are most likely to benefit. According to sources, tumors with high mutation load or high PD-L1 levels are more likely to respond to immune checkpoint therapy. - Combination therapies
Immunotherapy rarely stands alone; it is frequently combined with surgery, chemotherapy, radiation or targeted therapy. This approach is also evident in Dr Sudip’s practice, particularly when tumours are advanced or when conventional therapies alone may be insufficient. - Managing adverse effects and monitoring
Immune therapy may provoke immune-related adverse events (irAEs) since the immune system may attack normal tissues. Close monitoring, multidisciplinary collaboration (medical oncologist, endocrinologist, pulmonologist) and early intervention are essential standards of care actively maintained under Dr Sudip’s oversight.
Access, cost, patient counselling and local adaptation
In Nepal’s setting, cost, access to biomarker testing, infrastructure for safe delivery of immunotherapy and capacity for managing irAEs pose additional considerations. Dr Sudip’s role includes patient education, setting realistic expectations, and integrating immunotherapy into the wider oncology service with sustainability in mind.
Data and Evidence – Outcomes and Expectations
- According to a review article, the response rates of immunotherapy in some solid tumours range from about 15-30% in common solid tumours, and higher (45–60%) in certain cancers such as melanoma or those with MSI-high status.
- The literature highlights that head & neck squamous cell carcinomas (HNSCCs) are highly immunosuppressive malignancies with high mutational burden representing an area where immunotherapy research is active.
- Historical perspective reveals that the concept of cancer immunotherapy has been evolving for over a century, but the “modern era” of checkpoint inhibitors began in the last decade.
- It is important to note that immunotherapy is not effective in all cases. Numerous challenges remain: heterogeneity of tumour response, mechanisms of resistance, cost, access, and prediction of benefit.
Strengths and Limitations
Strengths:
- Ability to produce durable responses in a subset of patients.
- Potential for fewer direct toxicities than high dose chemotherapy in some settings.
- Possibility of re-educating the immune system to offer long term surveillance against recurrence.
Limitations:
- Only a fraction of patients respond; biomarkers are imperfect.
- Risk of immune‐related adverse events (which can affect skin, gut, lungs, endocrine organs).
- Cost and infrastructure requirements (immune monitoring, biomarker assays, infusion facilities).
- In many cancers, especially in resource-limited settings, access and affordability remain major issues.
- Only a fraction of patients respond; biomarkers are imperfect.
Future Landscape and Innovation
Emerging directions in immunotherapy include:
- New checkpoint targets beyond PD-1/PD-L1 and CTLA-4.
- Combination immunotherapies (e.g., checkpoint + targeted therapy + radiation).
- Personalized vaccines and oncolytic virus therapies.
- Adoptive cell therapies extended to solid tumours.
- Better biomarkers to predict response and tailor treatment.
In the Nepal context, building trial infrastructure and local data sets will be critical for sustainable implementation.
FAQs
Q1. Who is a good candidate for immunotherapy under Dr Sudip’s care?
Patients with advanced or recurrent cancers, whose tumours express relevant biomarkers (PD-L1, MSI-high, high tumour mutational burden) or who are not ideal candidates for conventional therapies may be considered. A full evaluation including pathology review, biomarker testing, overall health status and multidisciplinary discussion is undertaken.
Q2. What benefits can immunotherapy offer in the Nepal setting?
Under Dr Sudip’s management, benefits may include longer survival, improved quality of life, and potential for durable responses. The goal is to integrate immunotherapy into the broader care pathway (surgery, radiation, chemotherapy) to maximise outcomes.
Q3. What are the risks and how are they managed?
Risks primarily involve immune-related adverse events: inflammation of organs (lungs, liver, gut, skin, endocrine). Dr Sudip’s centre has protocols for early detection, management (often involving steroids, immunosuppressants), and multidisciplinary follow-up. Cost and monitoring are important considerations.
Q4. How is immunotherapy accessed and financed at the centre led by Dr Sudip?
Access involves assessment for biomarker testing, eligibility, cost-benefit discussion and insurance/assistance evaluation. The centre endeavours to ensure that patients receive treatment in a structured, safe environment. Local availability of drugs, infusion facilities and monitoring is arranged.
Q5. How does immunotherapy fit into the overall cancer treatment plan?
Immunotherapy is not a replacement for surgery, radiation or chemotherapy in most cases; rather it complements them. Under Dr Sudip’s care, the treatment plan is personalised: whether immunotherapy is given upfront, in combination, or as a salvage therapy depends on tumour type, stage, biomarker status and patient fitness.
Conclusion
The integration of immunotherapy into contemporary oncology practice underlines a shift from purely tumour centric treatment toward immunologic and systemic strategies. In the hands of a clinician like Dr Sudip Shrestha, who combines global oncology standards with local health system realities, this evolution holds promise for patients in Nepal. While challenges remain cost, biomarker access, patient selection the potential for meaningful benefit is real.
By aligning the latest evidence on immunotherapy with structured implementation, multidisciplinary care and patient centered counselling, the Nepal Cancer Hospital & Research Center under Dr Sudip is contributing to bringing advanced oncology into a regional context. As immunotherapy further evolves, continued local research, adaptation and capacity building will determine how widely those benefits extend.